A collaboration with a state health system to make tracking professional services easier for everyone
Objective
Discover barriers to consult tracking, culturally and systemically, and design a way to track consults that Public doctors will use.
Role
As the lead UX researcher and designer on this project, I worked with UI designers, project managers and developers to plan and conduct research and testing, as well as wireframing/concept development.
Brief–
In the Australian hospital system, public hospitals are government-funded. Private hospitals are available to those who have self-paid insurance or when necessary services are unavailable at a public hospital. In Sydney, a Private hospital (cancer-specific) sits across the street from a Public hospital (general).
Private vs. Public: the quest to recover funds.
Doctors and other personnel from the Public hospital are frequently asked to perform consultations at the Private hospital for complex conditions (cancer combined with other conditions, such as diabetes). The Public consultants do not track their time or other information about Private consults, so the Public hospital is losing money due to an inability to bill for time spent attending to Private requests. Past attempts to track, including paper timesheets and a person sitting near the doors to catch personnel coming and going, have been ineffective.
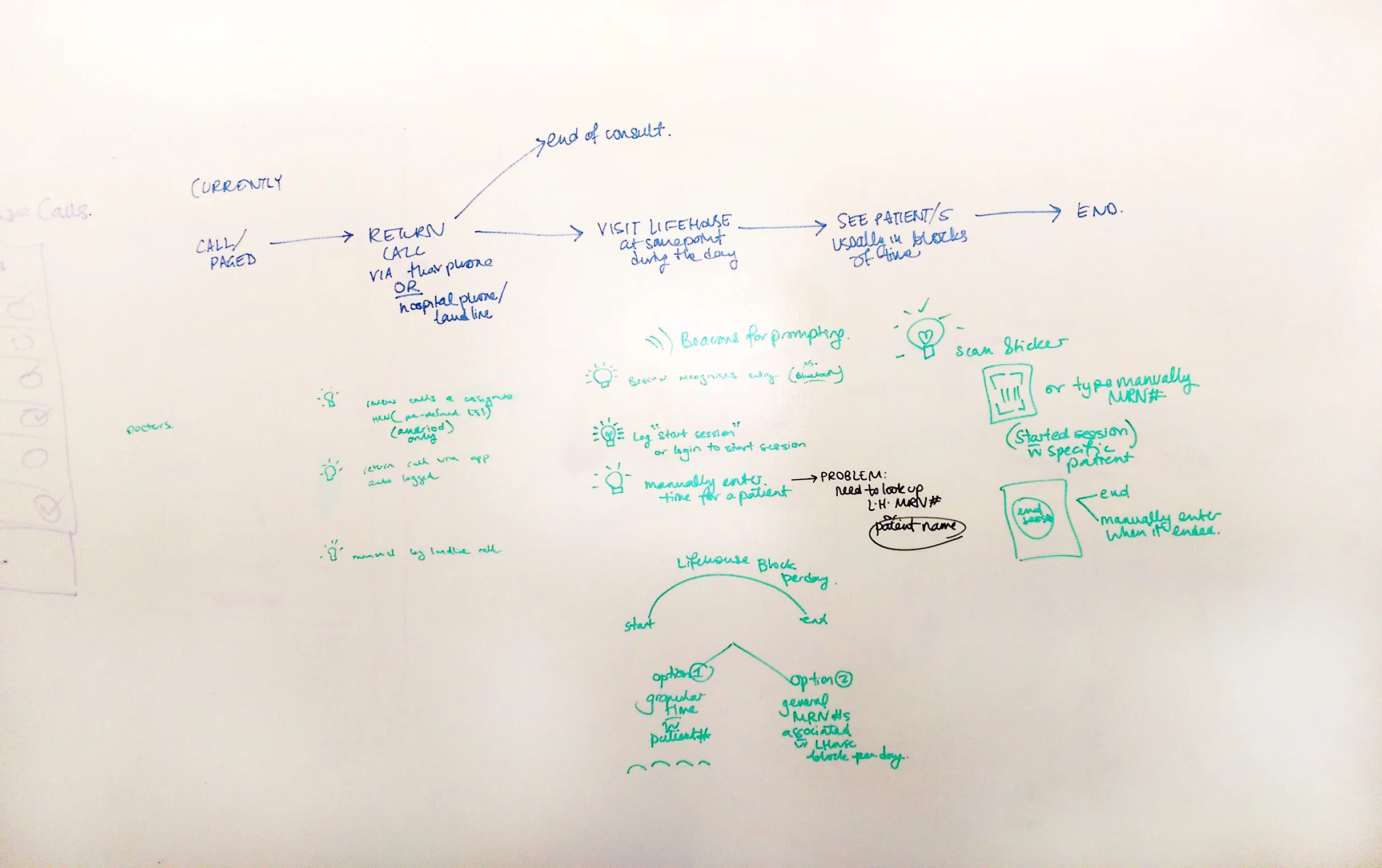
Brainstorming solutions for consult tracking.
Process–
After a brief stakeholder meeting to identify what information the Public hospital needed to gather, we interviewed groups of every type of user; Doctors, Residents, Nurses and Allied Health Professionals (e.g. Dietitians).
An example of a communal workstation in the Private hospital.
We learned that each group consulted with the Private hospital in a different way. Some visited infrequently, some every single day. Others completed many consults in one phone call. Some already tracked time for their specific department and others did not. When it came to receiving consult requests, disorganization was the main commonality among the groups, with requests coming through phone, text, email, even fax. With this information, we decided to shadow some of the users we interviewed to see a typical day with a consult.
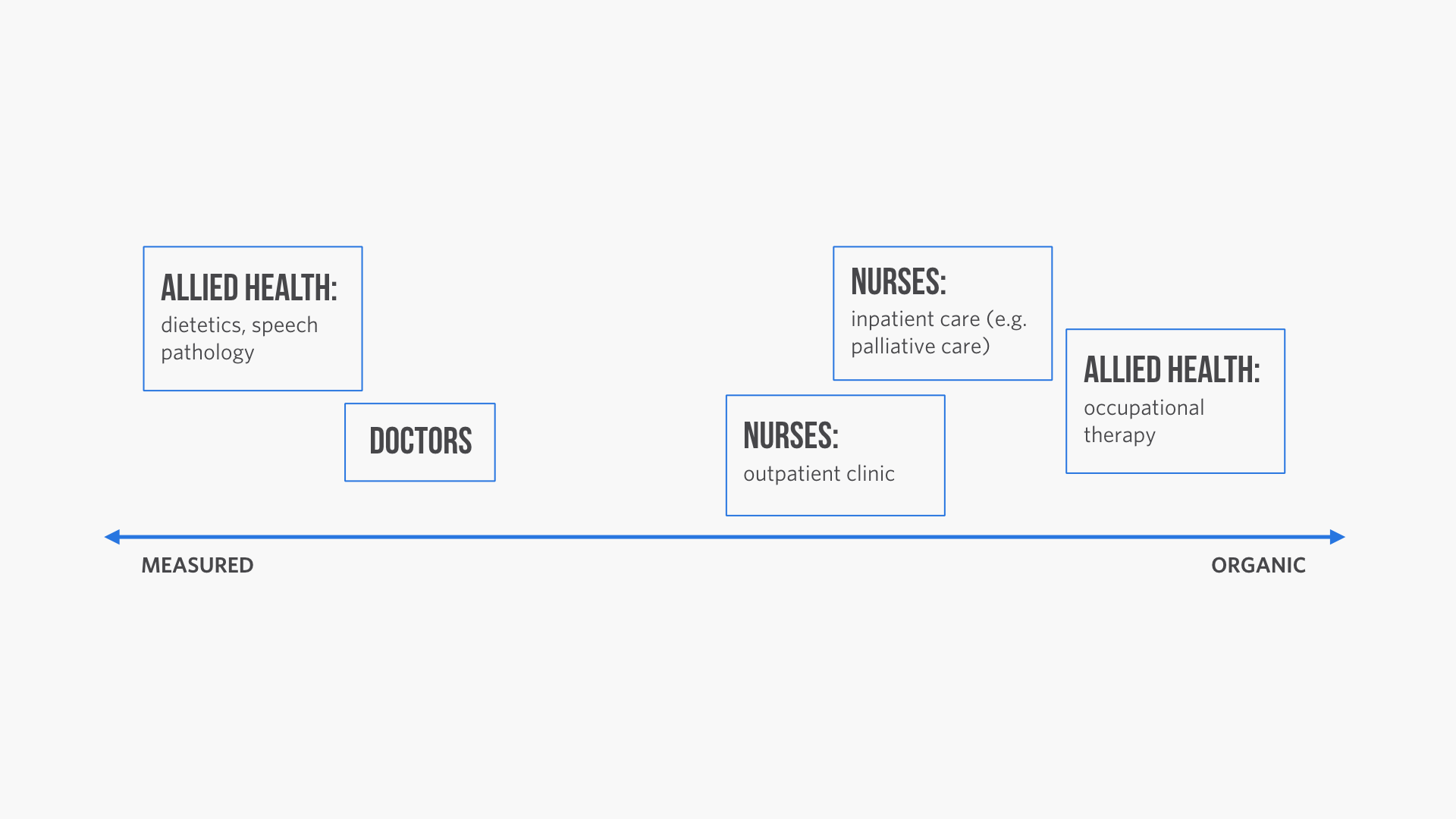
Not only did users have different job descriptions and varied access to technology–they also interacted with patients in unique ways.
The biggest takeaway from shadowing was that each type of user landed in a different place on the spectrum of measured interaction (appointments) to organic interaction (doing unscheduled rounds, being pulled into a consult when walking down the hall). When interaction was organic, users who tracked time tended to wait until the end of the day to try and estimate the length of their activities and who they saw; those with measured interaction usually tracked in the moment (using the computer in their office or a readily available paper chart). Users whose interactions were organic also complained of spending in excess of 45 minutes per day tracking down and filling in paperwork.
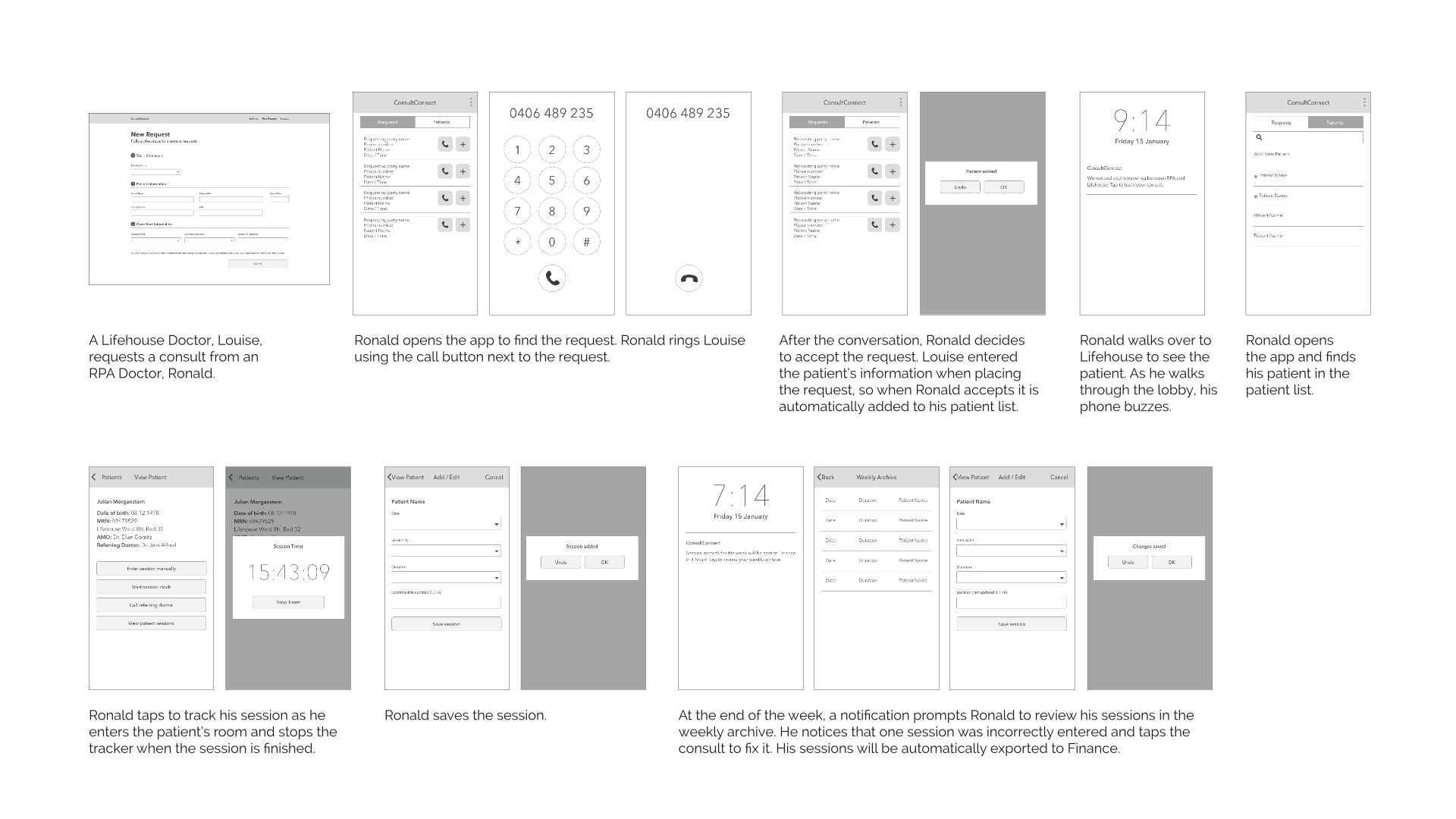
A flow explaining the tracking tool.
Results–
Our proposed solution responded to key issues discovered in our research:
- Tech put to good use. For Private requestors, the system is web based, and Public consultants use it on a tablet/mobile device (owned personally or by the hospital) to serve their in-motion work styles.
- Standardization of requests. In our solution, a Private requestor enters consult information through a web form, thereby standardizing the receipt of requests and capturing most patient information necessary for billing. There is no option to make requests outside of the form, so it captures virtually all consults.
- Tracking relevant to behavior patterns. When a Public consultant visits patients, he/she has the option to scan the patient’s chart sticker if the information is incomplete (this saves time and minimizes errors). The app is equipped with a consult timer function (essentially a stopwatch) to make it simple for users to track in the moment and a session timesheet for users who need to catch up on tracking at the end of the day.
- On-time delivery. At the end of each period, tracking records are automatically sent to each employee’s manager in .csv format, eliminating the need to fill out multiple timesheets. To show the concept, we produced an interactive prototype and tested it with users to gauge its usefulness and make improvements.
At the conclusion of the project, we delivered a low-fidelity prototype,* annotated wireframes* and screens to set the tone of the visual design.* The deliverables were well received and the app is in the pipeline for development.
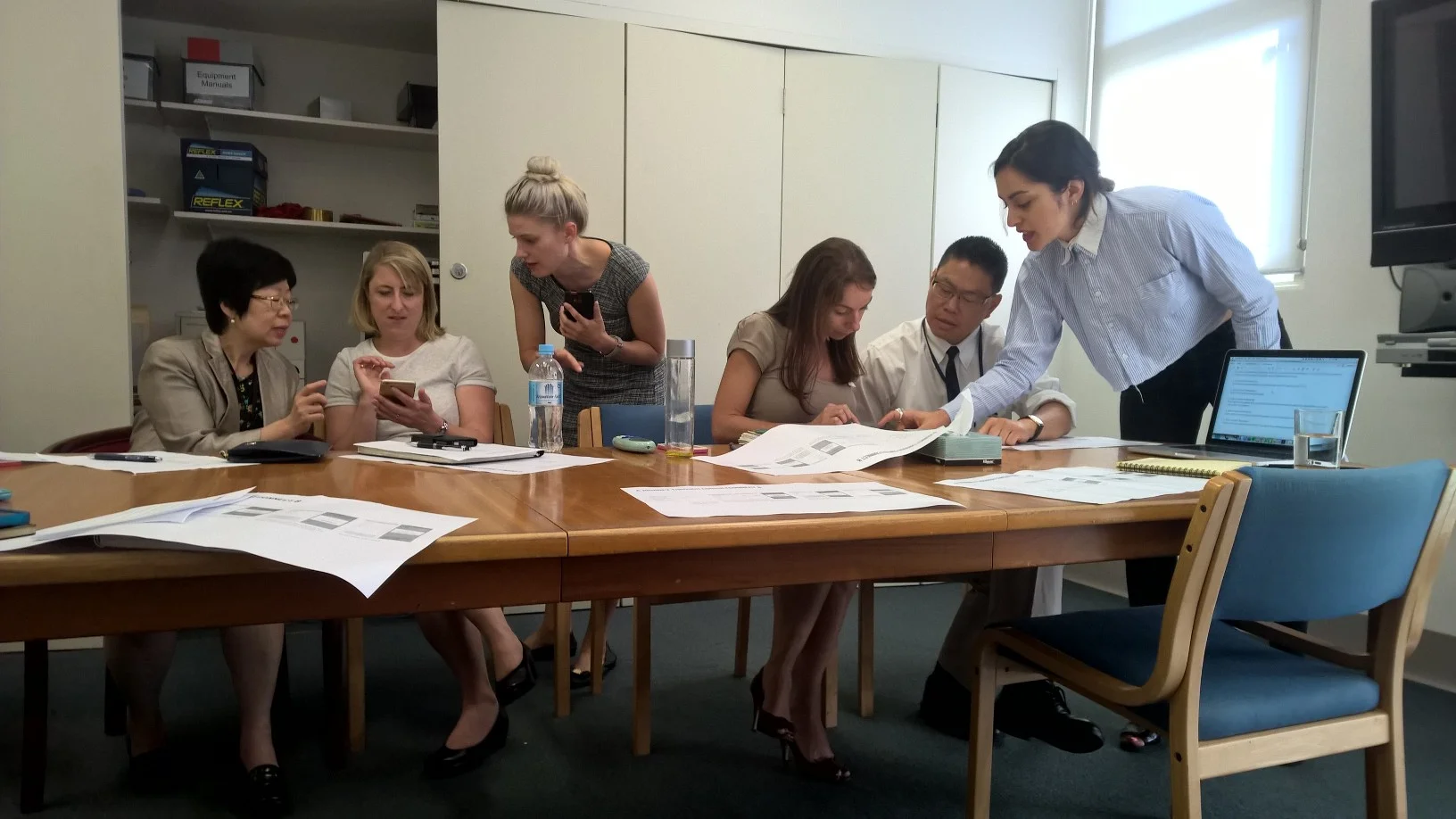
Taking feedback about a prototype after testing.
Obstacles–
The Public hospital refused to involve the Private hospital in user testing or meetings about this project for fear they would try to somehow stop the bills from coming. Since there was no validation from Private users of the solution, we developed a pared-down version of the app in addition to the proposed one, in which Public users imported patient information themselves.
The expectations for this project were very vague: the expected result was a solution for tracking time. Through research, we discovered that pagers and mobile devices were the things that doctors reliably had access to no matter what they were doing. Hospital administrators were open to purchasing mobile devices for departments that did not currently own them, so we decided an app for mobile devices would be most effective.